The three types of stoma are:
- Colostomy
- Ileostomy
- Urostomy
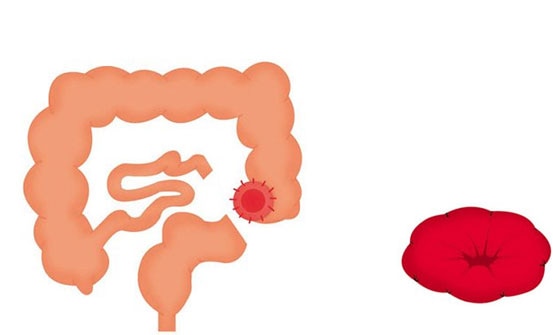 Colostomy
Colostomy
In a colostomy operation, part of the colon is brought to the surface of the abdomen to form the stoma. A colostomy is usually created on the left-hand side of the abdomen. Stools in this part of the intestine are solid and, because a stoma has no muscle to control defecation, will need to be collected using a stoma pouch.
There are two different types of colostomy surgery: End colostomy and loop colostomy.
End colostomy
If parts of the large bowel (colon) or rectum have been removed, the remaining large bowel is brought to the surface of the abdomen to form a stoma. An end colostomy can be temporary or permanent. The temporary solution is relevant in situations where the diseased part of the bowel has been removed and the remaining part of the bowel needs to rest before the ends are joined together. The permanent solution is chosen in situations where it is too risky or not possible to re-join the two parts of the intestine.
Loop colostomy
In a loop colostomy, the bowel is lifted above skin level and held in place with a stoma rod. A cut is made on the exposed bowel loop, and the ends are then rolled down and sewn onto the skin. In this way, a loop stoma actually consists of two stomas (double-barrelled stoma) that are joined together. The loop colostomy is typically a temporary measure performed in acute situations. It can also be carried out to protect a surgical join in the bowel.
Ileostomy
In an ileostomy operation, a part of the small bowel called the ileum is brought to the surface of the abdomen to form the stoma. An ileostomy is typically made in cases where the end part of the small bowel is diseased, and is usually made on the right-hand side of your abdomen.
Stools in this part of the intestine are generally fluid and, because a stoma has no muscle to control defecation, will need to be collected in a pouch.
There are two different types of ileostomy surgery:
|
End ileostomy
An end ileostomy is made when part of the large bowel (colon) is removed (or simply needs to rest) and the end of the small bowel is brought to the surface of the abdomen to form a stoma. An end ileostomy can be temporary or permanent.
The temporary solution is relevant in situations where the diseased part of the bowel has been removed and the remaining part needs to rest before the ends are joined together. The permanent solution is chosen in situations where it is too risky or not possible to re-join the two parts of the intestine.
|
|
Loop ileostomy
In a loop ileostomy, a loop of the small bowel is lifted above skin level and held in place with a stoma rod. A cut is made on the exposed bowel loop, and the ends are then rolled down and sewn onto the skin. In this way, a loop ileostomy actually consists of two stomas that are joined together.
The loop ileostomy is typically temporary and performed to protect a surgical join in the bowel. If temporary, it will be closed or reversed in a later operation.
|
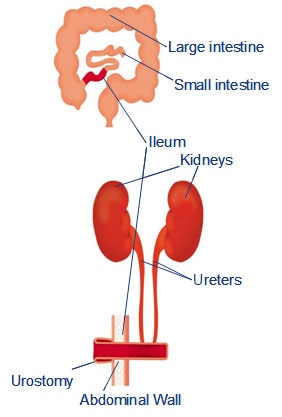 Urostomy Urostomy
If the bladder or urinary system is damaged or diseased and your patient is unable to pass urine normally, there is a need for a urinary diversion. This is called a urostomy, an ileal conduit or a Bricker bladder.
An isolated part of the intestine is brought onto the surface of the right-hand side of the abdomen and the other end is sewn up. The ureters are detached from the bladder and reattached to the isolated section of the intestine. Because this section of the intestine is too small to function as a reservoir, and there is no muscle or valve to control urination, your patient will need a urostomy pouch to collect the urine.
|